Drug Lesson #5: Lisinopril
I am back for another drug lesson! I enjoy doing these articles because it is helpful for the general public to understand the medications they are on. Additionally, I hope to explain medications to others who are not medically literate.

I am back for another drug lesson! I enjoy doing these articles because it is helpful for the general public to understand the medications they are on. Additionally, I hope to explain medications to others who are not medically literate.
Lisinopril is a commonly used medication for multiple cardiovascular conditions like high blood pressure and heart failure. It is the #3 most frequently prescribed medication in the United States, estimated at 91,862,708 prescriptions as of 2019.1 Today, I will present how lisinopril works and its side effects.
What is lisinopril?
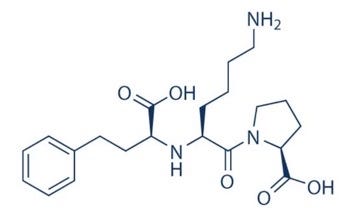
Lisinopril belongs to a class of medications called Angiotensin-Converting Enzyme Inhibitors (ACE-I’s). ACE-I’s inhibit the enzyme ACE, which plays a role in constricting blood vessels and maintaining blood pressure2. Using lisinopril will inhibit the constriction of blood vessels, thus decreasing blood pressure.
To explain how lisinopril works, I first have to introduce a compensatory system called the RAAS system in our body. RAAS stands for Renin-Angiotensin-Aldosterone-system. When the blood volume in our vessels decreases, this system is activated. A cascade of reactions occurs, which results in constriction of blood vessels and the kidneys retaining sodium and water in the body. This will maintain the blood volume in your body and maintain blood pressure.

Lisinopril inhibits the enzyme that converts angiotensin I to angiotensin II. This prevents the production of angiotensin II and its ability to bind to the angiotensin receptor and subsequent constriction of blood vessels. This is why lisinopril is used to treat those with high blood pressure.
When do we use it?
Lisinopril is FDA-indicated for use in high blood pressure, heart attacks, heart failure, and chronic kidney disease2. All ACE inhibitors are first-line medications for these disease states.
A 1991 trial studied the effect of enalapril (another ACE inhibitor) on survival in those with heart failure, and the study provided data supporting a mortality benefit with using enalapril3. This impacted the current heart failure guidelines created by the American Heart Association, stating that ACE inhibitors are first-line agents for those with heart failure with a proven mortality benefit.
What about the side effects?

All ACE inhibitors, including lisinopril, have the following side effects:
- cough
- headache
- swelling of the lips and face (angioedema)
- acute kidney injury
- low blood pressure (hypotension)
A dry, nonproductive cough is the most common side effect of lisinopril, occurring in up to 20% of patients.4 If the cough disrupts daily living, then switching to another blood pressure medication is appropriate.
When should a patient NOT be taking lisinopril?
There are particular populations where patients should not take lisinopril, and those include:
Hypersensitivity to ACE inhibitors Pregnant People
Those who are pregnant should be switched to a different blood pressure medicine due to the medication crossing the placenta and being associated with fetal malformations during the first trimester.5
Can pregnant people take lisinopril?

As stated above, ACE inhibitors should be discontinued as soon as pregnancy is detected. Other blood pressure medications have more safety data associated with maternal and fetal health.
Extra Tips!
- If you develop a dry, hacking cough during the first month of lisinopril therapy, notify your physician as soon as possible.
- Stop taking lisinopril if you develop hives or throat swelling, and seek medical attention.
- Notify your physician if there are any changes in your urine volume or color.
References
- https://clincalc.com/Drugstats/Drugs/Lisinopril
- Lisinopril Monograph, Lexicomp Medical
- “Effect of Enalapril on Survival in Patients with Reduced Left ….” N.p., n.d. Web. 1 Mar. 2022 <https://www.nejm.org/doi/full/10.1056/nejm199108013250501>.
- Bangalore S, Kumar S, Messerli FH. Angiotensin-converting enzyme inhibiinhibitor-associated: deceptive information from the Physicians’ Desk Reference. Am J Med. 2010;123(11):1016–1030. doi:10.1016/j.amjmed.2010.06.014
- “ACC/AHA guidelines for the evaluation and management of chronic ….” N.p., n.d. Web. 1 Mar. 2022 <https://pubmed.ncbi.nlm.nih.gov/11738322>.