The Antibiotic Ladder
When I was learning about antibiotics in school, it fried my brain. I felt like there were too many drugs to remember, especially when picking the correct one. One thing that helped me understand the algorithm behind antibiotics is the antibiotic ladder.
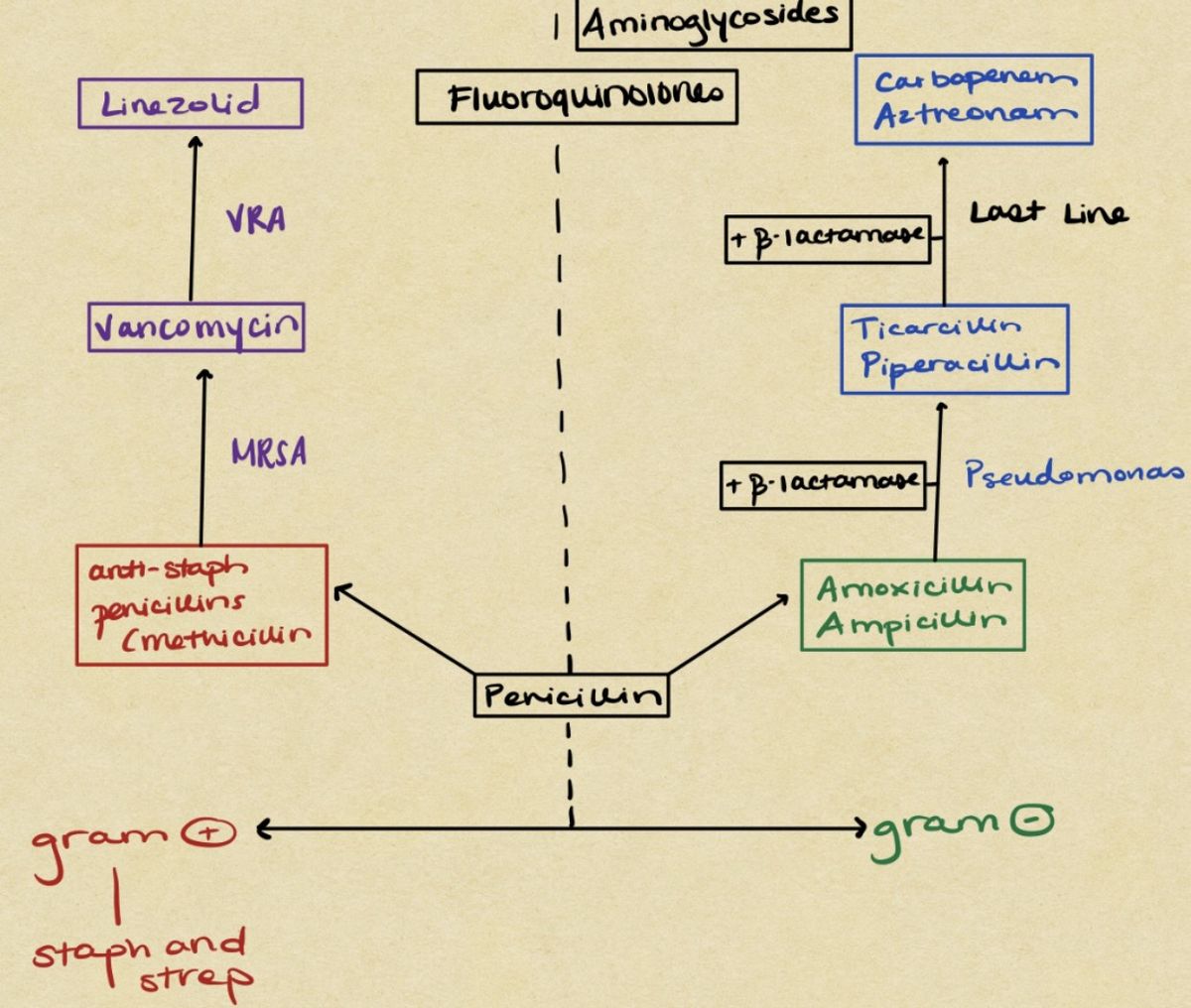
When I was learning about antibiotics in school, it fried my brain. I felt like there were too many drugs to remember, especially when picking the correct one. One thing that helped me understand the algorithm behind antibiotics is the antibiotic ladder. It’s a timeline of the discoveries of each antibiotic class. The higher up on the latter, the more narrow their target is. Additionally, the higher up the ladder, the less antibiotic resistance there is.
In this article, I will go through a few diagrams that aided me in school.
Penicillin
Penicillin is at the bottom of the ladder because it was the first beta-lactam discovered (1928). After almost one hundred years, bacteria have grown accustomed to resisting penicillin easily. Nowadays, penicillin has strict coverage over the streptococcus genus. From penicillin, the ladder branches out into gram-positive bacteria. (staphylococcus and streptococcus) and gram-negative bacteria.
Anti-Staphylococcal Penicillins
Next, starting from the left of the ladder, I will discuss bacteria with targeted gram-positive coverage. Since penicillin only covers strep, we need to find an antibiotic class that has staph coverage. The anti-staphylococcal penicillins come into play here. Examples of medications in this class include methicillin, oxacillin, nafcillin, and dicloxacillin.
Vancomycin
So now we have antibiotics that cover both strep and staph. Some staph bacteria will adapt to these antibiotics and become MRSA (methicillin-resistant staph aureus). These bacteria are resistant to the anti-staph penicillins. So how do we fix that?
Scientists developed vancomycin in the 1950s, and it targets MRSA. If a hospital confirms MRSA in a patient, they will start them on vancomycin. This medication can cover some other gram-positive bacteria, but its primary use is for MRSA.
Linezolid
After vancomycin, we’ve gotten to the last line for gram-positive bacteria. Scientists made Linezolid combat another resistant bacteria species: VRE (vancomycin-resistant enterococcus).
The most crucial point to remember with linezolid is that it is the last line, and use it when necessary. If resistance arises against linezolid, physicians don’t have a backup.
Gram-Negative Bacteria
Let’s shift to the other side of the ladder, starting with amoxicillin and ampicillin.
Amoxicillin and Ampicillin
To talk about these drugs, we first have to address penicillin. I mentioned before that penicillin only retains coverage for strep. Scientists realized this and created amoxicillin and ampicillin. These drugs cover gram-negative bacteria.

Soon after the discovery, bacteria started to resist amoxicillin and ampicillin. The way they accomplished this was through an enzyme called beta-lactamase. These enzymes reside in the cell membrane of bacteria. Their job is to inactivate beta-lactam antibiotics by breaking the beta-lactam ring.
How did scientists fix this? Well, a new class of medications targeting beta-lactamases combined with amoxicillin or ampicillin solved the problem. Some combinations include amoxicillin/clavulanate and ampicillin/sulbactam.
Pseudomonas Aeruginosa
Pseudomonas is a gram-negative rod responsible for multiple infections, including urinary tract infections, skin and soft tissue infections, and bacteremia¹. Pseudomonas infections are most prominent in patients who are hospitalized and have cancer or cystic fibrosis.
Broad Spectrum Beta-Lactams
Once pseudomonas became resistant to the beta-lactam/beta-lactamase combinations, physicians struggled to find a new class covering pseudomonas. This is where piperacillin and ticarcillin come in. These medications are broad-spectrum beta-lactam antibiotics that cover pseudomonas. They are often paired with a beta-lactamase inhibitor. Some examples include piperacillin/tazobactam and ticarcillin/clavulanate.
Carbapenems
When bacteria become resistant to piperacillin/tazobactam and ticarcillin/clavulanate, carbapenems are the last line for getting rid of these bacteria. Carbapenems cover resistant bacteria strains that produce ESBLs (extended-spectrum beta-lactamases). Examples of carbapenems include imipenem, ertapenem, and meropenem.
A word of caution with these medications: they are the last line for resistant gram-negative bacteria. Use them only when necessary because there is no backup option once bacteria resist carbapenems.
Aminoglycosides
Aminoglycosides are a class of antibiotics that work against only gram-negative bacteria. They have increased toxicity, especially in the kidneys and ears. They cover ESBL producing bacteria and pseudomonas. Examples of aminoglycosides include amikacin, gentamicin, and tobramycin.
Cephalosporins

Cephalosporins belong to the beta-lactam family and have five generations. The chart to the left explains their spectrum, which changes from generation to generation. First-generation cephalosporins are great for gram-positive bacteria but poor for gram-negative bacteria. As the generations go on, they lose gram-positive activity and gain gram-negative activity.
Examples:
- 1st generation: cefazolin, cephalexin
- 2nd generation: cefuroxime, cefoxitin, cefotetan
- 3rd generation: ceftriaxone, cefdinir, ceftazidime
- 4th generation: cefepime
- 5th generation: ceftaroline, ceftolozane
Fluoroquinolone Baseball Diamond

This diagram helps to remember which fluoroquinolones cover gram-positive and gram-negative bacteria. Starting from the left, moxifloxacin has excellent action against gram-positive bacteria. It is used to treat respiratory infections, abdominal infections, and skin infections.²
Levofloxacin has coverage against both gram-positive and negative bacteria. It is used to treat respiratory infections, pneumonia, and sexually transmitted diseases.³
Lastly, ciprofloxacin works against gram-negative and anaerobic bacteria. It is most commonly prescribed to treat urinary tract infections, osteomyelitis⁴, and pneumonia.⁵
Anaerobic Coverage

Physicians prescribe certain antibiotics that cover anaerobic bacteria very well. I don’t have a diagram for you, but I am a fan of acronyms. The one I came up with is MAP CCC. Remembering this acronym might help with remembering which antibiotics work against anaerobes.
Antibiotics are tough to learn but not impossible. I’m still working on remembering them, and these diagrams have helped me a lot. I hope they help you too.
Footnotes:
- bacteremia: the presence of bacteria in the bloodstream
- Moxifloxacin monograph, Lexicomp Medical
- Levofloxacin monograph, Lexicomp Medical
- Osteomyelitis: infection of the bone
- Ciprofloxacin monograph, Lexicomp Medical